Trésor-Economics No. 179 - What are the economic consequences of obesity and how to tackle them?
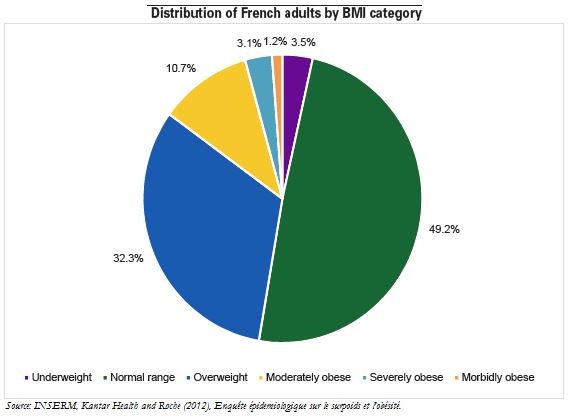
Overweight and obese people make up just under half of the French population, but they account for a disproportionate share of healthcare expenditure (56% for outpatient care and probably more for inpatient care). Excess bodyweight has particularly negative consequences for human health, raising morbidity by the heightened risk of chronic disease, and raising mortality, as 13% of deaths recorded in Europe in 2002 were attributed to obesity. Obesity also reflects major social inequalities, as it is disproportionately present among low-income households.
In France, the social cost of excess bodyweight was approximately €20 bn (1% of GDP) in 2012–an amount comparable to the social cost of alcohol and tobacco. The cost per individual concerned, however, is substantially lower than for alcohol or smoking, because far more people are overweight. Furthermore, individual behaviours must not be stigmatised because-unlike alcohol and tobacco, which are matters of individual behaviour–obesity has multiple causes, such as the quality of food consumed and genetic factors.
While appropriate actions have been undertaken in an attempt to limit the rise in the number of overweight people, they appear inadequate in light of the health risks involved, and more specifically the projected increase in the number of obese and overweight people (in France, 33.0 million in 2030, up from 24.6 million in 2012). In the past, prevention has focused on mass media campaigns. Measures could be taken both to strengthen incentives for physicians to expand prevention, and to make nutritional taxes more effective in changing behaviours.
While behavioural taxation can be a welcome instrument in improving anti-obesity policies in France, other, innovative and economical anti-obesity measures could be promoted, including:
- focusing on "unconscious" incentives in consumer decision-making, to bring about a healthier diet;
- better-targeted prevention campaigns;
- restricting or even banning advertising targeted at children for products whose overconsumption can be unhealthy;
- strengthening nutritional labelling requirements.
Lastly, organising intensive counselling of obese people by healthcare professionals appears to be highly promising but potentially costly in the short term. Two factors make such counselling difficult: lack of incentives for physicians and lack of resources in regions with low physician-to-population ratios.